GD Topic - Monkeypox Outbreak: A Wake-Up Call for Better Disease Surveillance
Candidates planning to pursue MBA must prepare for the Group Discussion Round as it can make or take the chances of admission. Check out the article below for a discussion on the GD topic: Monkeypox outbreak. Learn about the disease, its symptoms, the 2022-24 outbreak, and its current status.
What truly defines a future business leader—stellar academic scores or the ability to think critically, communicate effectively, and lead with confidence? In the competitive world of MBA admissions, the Group Discussion (GD) round holds the answer. Apart from the numbers achieved in MBA entrance exams like CAT, XAT, SNAP, NMAT, and MAH MBA CET, the GD round evaluates candidates on essential skills such as communication, leadership, confidence, analytical thinking, and time management. In a GD round, a group of aspirants discusses a given topic within a set timeframe (20-25 minutes). GD is conducted to identify individuals who can effectively collaborate, persuade, and present their viewpoints—traits that every top B-school values in its future managers.
With MBA entrance exams going on, candidates planning to get admission in top B-schools like IIM, XLRI Jamshedpur, SBIM Pune must start preparing for the GD round. As of now, the Group Discussion (GD) round for CAT is ongoing, while GD rounds for other entrance exams are expected to conclude by February 2025. This timeline shows the importance of prompt preparation for candidates wanting to shine in their interviews and GD. Read the below article for a discussion on one of the important current GD topics; the Monkeypox Outbreak.
Check Out: Top MBA Colleges in India
The monkeypox outbreak is a clear reminder for everyone that the world remains vulnerable to emerging infectious diseases, even after the devastating COVID-19. The pandemic taught us the importance of having strong health systems; however, the rapid spread of monkeypox shows that there are still gaps in how we monitor and respond to outbreaks. Post-COVID, the global community promised to be better prepared for future outbreaks, yet the monkeypox crisis exposed the lack of faster disease tracking and coordination. It shows the need for the world to use the lessons from COVID-19 to improve how we detect and control diseases, provide fair healthcare access to everyone, and build a stronger public health system to prevent future crises.
Before we indulge in the need for a better healthcare system, let us first understand what exactly is Monkeypox and its symptoms.
What is Monkeypox?
Mpox or Monkeypox is a rare viral disease caused by the monkeypox virus, a member of the Orthopoxvirus genus in the Poxviridae family. Mpox is closely related to smallpox, but it is less sever and generally less contagious. It is a zoonotic disease, which means that the disease spreads from animals to humans. However, Mpox can also spread from human to human. Monkeypox is considered an emerging infectious disease and has gained global attention in recent years due to its outbreak outside its usual endemic regions.
Monkeypox was first identified in 1958 in monkeys kept for research and this how the disease got its name. However, monkeys are not the primary carriers of the virus. It is primarily found in certain rodents, such as squirrels and rats, which serve as the natural hosts. The first human case of monkeypox was recorded in 1970 in the Democratic Republic of Congo (DRC). A child was diagnosed with monkeypox when the world was trying to eradicate smallpox. Since then, monkeypox has been endemic to certain parts of Central and West Africa, particularly in countries like Nigeria, Cameroon, and the DRC.
Types of Mpox (Monkeypox)
The monkeypox virus (Mpox or MPXV) has two primary genetic clades; Clade I and Clade II, which are further divided into subclades. The clades are distinguished based on their geographic origins, severity, and transmission characteristics.
- Clade I (Central African Clade):
- Clade Ia: This clade is primarily found in endemic areas within the Democratic Republic of Congo (DRC). Clade Ib transmits more efficiently through human-to-human contact compared to other clades. It involves high risk due to severe disease symptoms and 6-10% mortality rates.
- Clade Ib: This clade affects non-endemic regions in the DRC and neighboring countries. It is also classified as high-risk and has caused an increase in cases due to emerging networks of transmission, including sexual contact.
- Clade II (West African Clade)
- Clade IIa: This subclade is found in endemic regions such as Nigeria and other West and Central African countries, and causes milder disease symptoms compared to Clade I. The mortality rate of Clade IIa is lower; 1-3%. Also, its transmission is less efficient compared to Clade I.
- Clade IIb: This subclade is seen outside endemic regions, especially in non-endemic countries in Europe, Asia, and the Americas. It is considered as moderately risky and has been seen during 2022 and 2024 outbreaks. The cause of its transmission is human-to-human close physical or sexual contact.
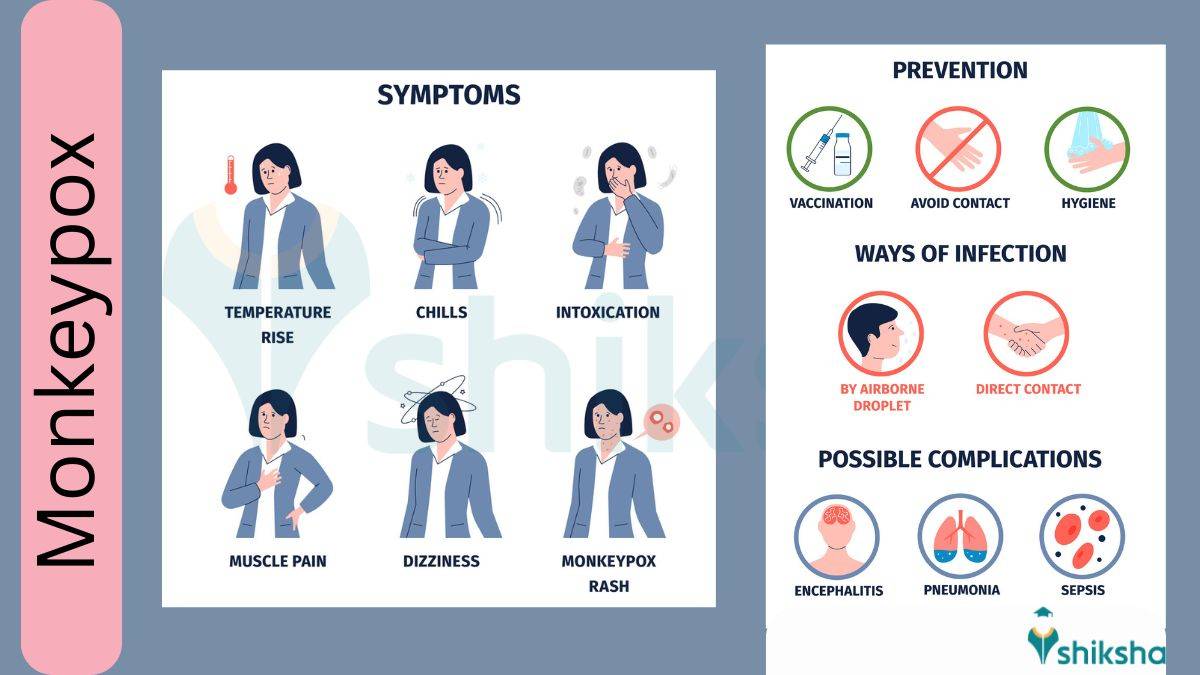
Signs and Symptoms of Monkeypox
Monkeypox symptoms usually appear within 1 to 21 days after exposure to the virus, known as the incubation period. The illness typically lasts for 2 to 4 weeks. These symptoms can range from mild to severe, depending on the individual’s health and the strain of the virus.
Common Symptoms of Mpox include:
- Rash
- Fever
- Sore Throat
- Headache
- Muscle Aches
- Back Pain
- Low Energy
- Swollen Lymph Nodes
For some people, the rash is the first symptom, while for others it may be fever, muscle ache, or a soar throat.
Mpox Rash
The mpox rash can begin on the face and then spread to other parts of the body, such as the palms of the hands, soles of the feet, and groin, or it may start in areas where the contact occurred such as genital areas.
It progresses in stages:
- Flat sores (macules): Small, red spots on the skin.
- Raised bumps (papules): The sores become elevated.
- Blisters (vesicles): Fluid-filled bumps that may itch or cause discomfort.
- Pus-filled lesions (pustules): The blisters become filled with yellowish pus.
- Crusting and healing: The lesions dry up, scab over, and eventually fall off, leaving a new layer of skin underneath.
The number of lesions can vary between individuals. Some people may have just a few sores, while others may develop hundreds. These lesions can appear anywhere, including:
- Face, mouth, and throat
- Palms of the hands and soles of the feet
- Groin and genitals
- Anus
Severe Symptoms and Complications
In severe cases, mpox can lead to significant complications, such as:
- Painful swelling of the rectum (proctitis) or difficulty urinating (dysuria).
- Bacterial skin infections, which may result in abscesses or permanent skin damage.
- Respiratory issues: Including pneumonia or difficulty breathing.
- Eye infections (keratitis or corneal infection): Potentially leading to vision loss.
- Digestive problems: Vomiting and diarrhea, causing dehydration or malnutrition.
- Serious infections: Such as sepsis, brain inflammation (encephalitis), heart inflammation (myocarditis), and infections of the urinary or genital organs.
High-Risk Groups
Individuals who are at a higher risk of severe illness or death from monkeypox, include:
- Children
- Pregnant Women
- People with weak Immune System (such as those living with uncontrolled HIV or undergoing treatments that suppress immunity)
2022-2024 Monkeypox Outbreak
The monkeypox outbreak in 2022 was the first large-scale spread of the disease outside its usual endemic regions in Central and West Africa to non-endemic countries across Europe, North America, South America, Asia, and the Middle East.
The first case of the 2022 outbreak was reported in the United Kingdom in May, and by August 2022 over 14,000 laboratory-confirmed cases were reported globally, signaling the start of a global health concern. In India, the first monkeypox case was detected on July 14, 2022, when a traveler from the UAE, who had returned to Kerala, developed symptoms. This marked India's entry into the global outbreak, with subsequent cases being reported in various states, particularly among individuals with a history of international travel.
The rapid spread of monkeypox in 2022 was due to human-to-human transmission through close contact with infected individuals, respiratory droplets, or contaminated objects. Earlier, monkeypox spread through animal-to-human transmission in forested areas; however, the 2022 outbreak highlighted the potential for global spread due to increased international travel and social gatherings.
As cases increased worldwide, the World Health Organization (WHO) declared monkeypox a Public Health Emergency of International Concern (PHEIC) in July 2022. With PHEIC, the World Health Organization emphasized the urgent need for coordinated global action. The Indian government also increased its surveillance, issued guidelines for healthcare facilities, and educated people about the symptoms and preventive measures of monkeypox. By May 2023, the PHEIC was declared over after WHO saw a decline in global cases.
In DRC, monkeypox has been reported for more than a decade and the number of reported cases increased every year. In 2023, the number of reported cases increased significantly, and by mid-August 2024, the number exceeded the previous year’s total cases by more than 15,600 cases and 537 deaths. Due to the emergence and rapid spread of a new virus strain, clade 1b through sexual networks in DRC and its detection in its neighboring countries, on 14 August 2024 the World Health Organization (WHO) Director-General declared monkeypox a Public Health Emergency of International Concern (PHEIC) under the International Health Regulations (2005).
At the time, the World Health Organization (WHO) was actively working to ensure equitable access to vaccines for mpox, particularly in lower-income countries that have not yet issued their own national regulatory approvals. Two vaccines were in use on WHO’s Strategic Advisory Group of Experts on Immunization recommendation. WHO-listed national regulatory authorities and individual countries also approved these vaccines.
To speed up vaccine access, the Director-General of WHO also initiated the process for Emergency Use Listing (EUL), allowing for faster approval and procurement by global partners such as Gavi and UNICEF. In addition, WHO coordinated efforts with vaccine manufacturers and partners through the interim Medical Countermeasures Network to ensure the equitable distribution of vaccines, therapeutics, diagnostics, and other critical tools. Since then, WHO has been working with affected countries and partners to control these outbreaks.
Current Situation of Monkeypox
In November 2024, WHO conducted the latest global mpox rapid risk assessment. According to the gathered information, the risk of monkeypox was assessed as follows:
- Clade Ib MPXV: This clade is predominantly affecting non-endemic areas, including the Democratic Republic of the Congo (DRC) and neighboring countries, and is considered to pose a high risk.
- Clade Ia MPXV: This clade, primarily circulating in endemic regions within the DRC, is also categorized as high-risk.
- Clade II MPXV: It is observed in countries such as Nigeria and other areas in West and Central Africa, and is assessed to present a moderate risk.
- Clade IIb MPXV: This clade is associated with the ongoing global mpox epidemic, and is also deemed to have a moderate risk.
Monkeypox Cases: Statistics
As per the data reported to WHO by November 30, 2024; since January 1, 2022, 127 member states across all 6 WHO regions have reported cases of mpox to WHO. Additionally, 117,663 laboratory-confirmed cases and 2 probable cases, including 263 deaths have been reported to WHO. As of November 2024, compared to the number of reported monthly cases in October, the number of cases in November has decreased by 13.2%.
The 10 most affected countries globally since January 1, 2022, till November 2024 include:
- United States of America (34,349 cases)
- Brazil (13,236 cases)
- Democratic Republic of the Congo (10,492 cases)
- Spain (8,443 cases)
- France (4,371 cases)
- Colombia (4,280 cases)
- Mexico (4,192 cases)
- The United Kingdom (4,146 cases)
- Germany (4,040 cases)
- Peru (3,949 cases)
These countries collectively constitute 77.8% of the total cases reported globally.
Check Out Total Mpox cases by WHO region from 1 Jan 2022, as of 30 Nov 2024 at WHO’s official website
From 2024, as of January 12, 2025, 21 countries have reported 15,094 confirmed cases, including 64 deaths to WHO. The three countries with the most number of cases from 2024 include the Democratic Republic of the Congo (DRC) with 9513 cases, Burundi with 3116 cases, and Uganda with 1,830 cases.
Conclusion
The monkeypox outbreak has revealed significant gaps in global healthcare systems, particularly in disease surveillance and access to medical facilities. Many regions, especially low-income and underserved areas, continue to struggle with inadequate resources, making them vulnerable to such emerging health crises. This outbreak shows the urgent need for better systems for fast detection and response to diseases, along with fair access to healthcare and vaccines.
To prevent future outbreaks, global health authorities, like WHO must focus on strengthening healthcare systems, invest in early detection technologies, and foster international collaboration. By solving these issues, we can create a safer world that is better prepared to fight new diseases.
Top GD Topics for MBA Admission Process
Below listed are some of the important GD Topics for reference.
- Importance of Statue of Unity
- Citizenship Amendment Act - What and Why
- Making Aadhaar mandatory is not a good idea- for or against
- Implications of CAA-NCR
- Cashless Economy – Is India ready for it?
- All you need to know about Right To Information
- How can we control banking frauds to reduce NPAs?
- Statue of Unity - Symbol of Pride or Wastage of Public Money?
- Rural vs Urban India
- Environment and us
- Self Motivation
- First impression is the last impression
- Funding Democracy: Are Electoral Bonds a Boon or Bane?
- Quick Commerce: A Step Toward Progress or a Wasteful Luxury?
- Crime Against Women in India: Who Bears the Responsibility?
- Innovation Vs Invention: What does the world need?
- PM Internship Scheme: How Effective is it in Enhancing Youth Employability?
- Job Reservation in Private Sector: A Boon or a Barrier?
- Bharatiya Nyaya Sanhita (BNS): Reforming Criminal Law for Better or Worse?
- Electric Vehicles (EVs) in India: Dream or Reality?
- India’s Historic Performance at the Paris Paralympics 2024
- Global Innovation Index 2024: India Jumps from 81st to 39th Rank in 9 Years
- UCPMP 2024: Strengthening Ethical Standards in Pharmaceutical Marketing
- Global Food and Hunger Crisis: India Ranks 105 at Global Hunger Index 2024
- Making India a Semiconductor Powerhouse: The SEMICON India Programme
- Union Budget 2024: Are the New Income Tax Slabs a Win for the Middle Class?

Nupur is an experienced content writer with a specialized focus on Commerce students. Over the past three years, she has crafted engaging and insightful materials to help learners excel in their studies. Outside of ... Read Full Bio